Abstract
Background: Myelodysplastic syndrome (MDS) is a clinically heterogenous disease of hematopoietic stem cells characterized by peripheral blood (PB) cytopenias due to ineffective hematopoiesis in bone marrow (BM). Patients face increased morbidity from infection and/or bleeding, while having a high propensity for leukemic transformation. It is evident that aberrant chromosomal and genetic lesions are the key drivers of MDS pathogenesis, which also contributes towards chronic activation of the innate immune response and a hyperinflammatory BM microenvironment (Barreyro et al, Blood, 2018). Various types of immune cells like monocytes, dendritic cells, myeloid-derived suppressor cells (MDSCs), T cells, and NK cells also add to the aberrant cytokines within the BM microenvironment. In hematological malignancy, altered frequencies of monocytes, granulocytes, and MDSCs are well documented. Thus, in-depth understanding of this alteration is critical in order to provide clues about its role in MDS progression and develop targeted immunotherapies.
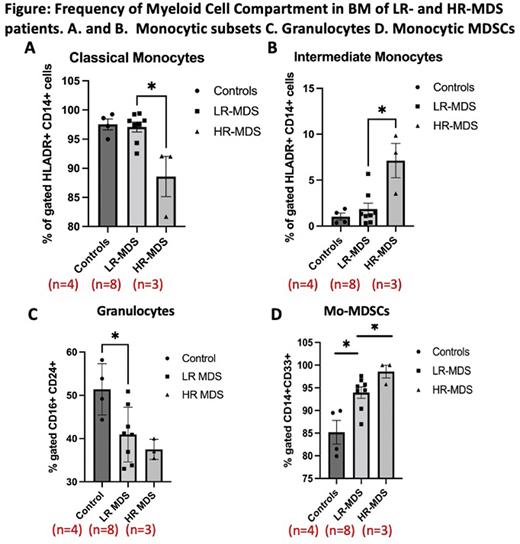
Method: BM myeloid cell compartment of MDS patients (n=11) was profiled by mass cytometry (CyTOF) and compared with age-matched healthy controls (n=4). Patients were further categorized into Low-risk (LR) MDS (n=8) and High-risk (HR) MDS patients (n=3) based on the IPSS-R score. All the patients included in this study were treatment naïve.
Result: Immunophenotypically, we were able to differentiate three subsets of monocytes: classical (CD14+/brightCD16+), intermediate (CD14+/brightCD16+) and non-classical monocytes (CD14dimCD16+). HR-MDS patients showed a significantly reduced proportion of classical monocytes (p<0.05) and a higher proportion of intermediate monocytes (p<0.05) compared to LR-MDS patients and healthy individuals (Figure A and B). However, the frequency of classical and intermediate monocyte subsets was comparable in healthy individuals and LR-MDS patients (Figure A and B). The proportion of non-classical monocyte was not statistically significant in LR-MDS and HR-MDS (data not shown). Furthermore, LR-MDS patients demonstrates reduced granulocyte frequency as compared to healthy individuals, HR-MDS patients shows lower frequency compared to LR-MDS patients, but the difference was not statistically significant (Figure C). We also observed a significant increase in the expansion of Mo-MDSCs from healthy individuals to LR-and HR-MDS patients (p<0.05) (Figure D).
Conclusion: Increased frequency of intermediate monocyte and Mo-MDSCs in HR-MDS patients points towards a hyperinflammatory phenotype and immunosuppressive microenvironment in HR-MDS patients which may facilitate the immune escape of blast cells and MDS progression. Additional studies are underway to further characterize the immune landscape in treatment-naive and treated MDS patients and to study the interaction of different immune components with blast cells.
Disclosures
Silverman:Celgene/BMS: Research Funding; Takeda: Research Funding; Gilead/Forty-Seven: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal